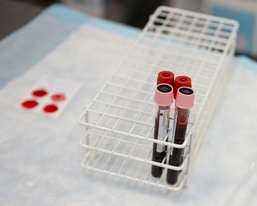
AL UDEID AIR BASE, Qatar— Al Udeid Air Base shipped its first unit of cold storage platelets on Aug. 17 to a location within the U.S. Air Forces Central Command Area of Responsibility. The shipment marked the first time cold storage platelets have been stored and shipped from Al Udeid Air Base for use in the AOR.
The platelets were collected from a volunteer donor and processed by the Apheresis Element here on Aug. 16.
“This is huge for the war fighter,” said U.S. Air Force Capt. Becky Pederson, chief assigned to the Apheresis Element of the 379th Expeditionary Medical Group.
Pederson explained that CSP is a new technique involving the handling, storage and shipment of platelets. By authorizing the use of CSP for DoD purposes outside of the United States, U.S. Central Command has made it possible to ship platelets to remote locations where they have not been available in the past. The current standards for handling platelets, approved by the U.S. Food and Drug Administration, known as room temperature platelets, require platelets to be stored at room temperature, limiting the shelf life to five to seven days and requiring constant agitation making it nearly impossible to ship to locations where equipment and access is limited.
The process for CSP has many advantages over the current FDA approved room temperature method. While room temperature platelets are susceptible to bacterial contamination, CSP are stored in a refrigerated environment with the likelihood of bacterial contamination nearly eliminated. In addition, RTPs must sit for 24 hours before they can be tested for bacteria prior to shipment, further limiting the viable shelf life of the product. CSP, on the other hand, can be tested within one hour of collection and shipped in a cooler the same day, possibly arriving to the field hospital with eight or nine days of shelf life.
“It changes the entire strategy for transfusions; I think it’s a very exciting development,” said Capt. Timothy Sommerville, internal medicine doctor assigned to the 379th EMG, referring to the use of CSP. “I think it has the potential to really move field medicine closer in line with the standard of care in the United States.”
There are two general options for treating a patient with significant blood loss. A doctor can conduct a transfusion using whole blood or use blood component therapy.
“Component therapy is a gold standard,” said Pederson. Safer than using whole blood, component therapy is the most commonly accepted method for conducting blood transfusions.
Packed red blood cells and blood plasma have been available in the field for some time and now CSP gives doctors all the components they need to use blood component therapy in trauma centers across the AOR. Blood component therapy refers to the procedure where blood is delivered to a patient in three separate components; packed red blood cells, blood plasma and blood platelets.
Blood used in whole blood therapy is available in two forms. The first form consists of pre-packaged units collected from donors, which are shipped and stored under refrigerated conditions. The second and more common form in battlefield conditions, explained Sommerville, is whole blood collected from a “walking blood bank” or, in other words, someone with the right blood type who is willing to donate then and there. The problem with a walking blood bank, however, is that although you get a fresh supply of vibrant blood, rejection is always a real possibility when using whole blood.
“There is almost no situation within the United States in which we would give whole blood,” said Sommerville. He goes onto explain that whole blood therapy is generally outdated and only used when component therapy is not an option.
“Most facilities down range do not have the capability to store platelets,” said Pederson, in reference to the FDA approved method of platelet storage.
Blood platelets are collected through the process of apheresis, which lasts approximately two hours. During that time, the donor’s blood is removed through a needle inserted in the vein above the elbow. The blood is circulated through an apheresis machine, where the platelets are separated out and the blood, minus the platelets, is returned to the donor. The process is comfortable and safe and most donors leave feeling great and generally unaffected by the donation.
It is very likely that CSP, a method developed by the military to advance the capabilities for saving lives in the field, will eventually be the standard practice used around the world for handling and shipping platelets.
“It’s a game changer, that’s for sure,” said Sommerville.